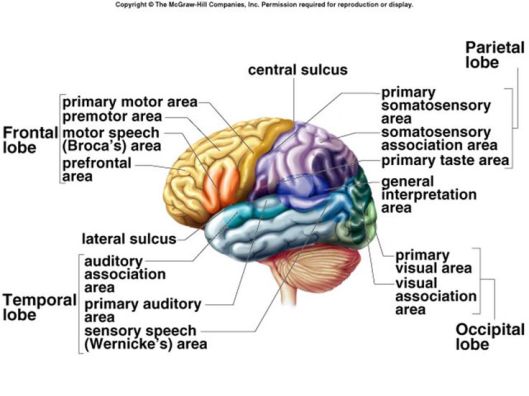
“Frontotemporal dementia (FTD) or frontotemporal degenerations refers to a group of disorders caused by progressive nerve cell loss in the brain’s frontal lobes (the areas behind your forehead) or its temporal lobes (the regions behind your ears)”
Also known as Pick’s Disease, FTD differs from Alzheimer’s Disease in various areas, but most noticeably in age (FTD comes at a younger age) and FTD does not necessarily involve the memory loss which makes Alzheimer’s so noticeable. For a more detailed look at the distinctive testing on FTD see here. As a general matter,
The frontal lobes, situated above the eyes and behind the forehead both on the right and left sides of the brain, direct executive functioning. This includes planning and sequencing (thinking through which steps come first, second, third, and so on), prioritizing (doing more Important activities first and less important activities last), multitasking (shifting from one activity to another as needed), and monitoring and correcting errors.
FTD is also correlated to “bad” even criminal behavior:
In addition to the inclusion of social cognition as one of the six domains potentially impaired by an NCD, forensic practitioners will be encouraged to note that legal involvement is specifically mentioned as one of the potential sequelae of frontotemporal NCD (Ref. 5, p 617). Behavioral and personality changes, including criminal acts and violations of social norms, are not uncommon in frontotemporal dementia (FTD). For example, a recent article in The Journal described several examples of aberrant and criminal behavior in a series of subjects who were subsequently found to have FTD. These included repetitive shoplifting despite the ability to pay, attempted child molestation, and hit-and-run. The relatively early age at onset and often, preserved memory and other abilities in FTD can make these types of cases challenging to explain to family members, victims, and courts as being due to organic disease rather than willful bad behavior. The new language concerning this diagnosis may help in explaining FTD and its effects to those involved.
DSM-5 and Neurocognitive Disorders
This leads to the question of the relationship between the brain damage and the behavior. If the brain damage causes the behavior, then why does the behavior differ so radically from person-to-person? The variety of bad acts suggest perhaps a variety of causes. Does the loss of executive function mean that previously existing inclinations are “permitted”? Since each instance of FTD would not be precisely the same, the difference stem from the difference in the area of the brain damaged? Do the people who have such damage act completely without restraint? If someone is shop lifting do they attempt to hide their acts — which would indicate an awareness of the “wrongness” of the activity. Can people who have such a condition rely upon an “external brain”, such as is suggested for people with FASD?
The cases reported seem to indicate a continued moral awareness:
Despite cognitive deficits, he had sufficient cognition to recall and understand his behavior and its wrongfulness. His lack of empathy and disinhibited compulsive tendency appeared to drive his pedophilic behavior. He was started on paroxetine 20 mg, divalproex 500/750 mg, and conjugated estrogens 0.625 mg. With this medical regimen and increased supervision, the patient had significant behavioral improvement. His case was not prosecuted.
And:
On being confronted, he recalled his egregious behaviors in detail, described them as inappropriate, and understood why he got into significant trouble because of them.
When the actor understands that his behavior is wrong, and has brain damage, how do we rightly judge the quality of his moral conduct?

Sometimes I think you are a Pastor, Lawyer, Biblical counselor, professor and Neuroscience scientist
Reblogged this on Talmidimblogging.
Thanks
You’re very welcome
Pingback: Frontotemporal dementia (FTD), Aberrant Behavior, and Moral Culpability — memoirandremains – THE BIG BUCK HUNTER 2018